Recognizing the Symptoms of Amyloidosis and Why Early Detection is Essential
Understanding Amyloidosis: An Overview
Amyloidosis is a rare but serious condition that occurs when an abnormal protein called amyloid builds up in organs and tissues throughout the body. This protein accumulation can interfere with the normal function of organs, such as the heart, kidneys, liver, spleen, and nervous system. Amyloidosis can be systemic, affecting multiple organs, or localized, impacting a single organ. The complexity of this condition lies in its variety of forms, each with distinct causes and implications.
Among the several types of amyloidosis, AL (light chain) amyloidosis is the most common. It is caused by an abnormality in plasma cells, which are responsible for producing antibodies. AA amyloidosis, another form, is linked to chronic inflammatory diseases. Hereditary amyloidosis, as the name suggests, is a genetic form of the disease.
Understanding the nature of amyloidosis is crucial for diagnosis and treatment. Due to its rarity and the overlap of symptoms with other conditions, amyloidosis often goes undiagnosed until significant organ damage has occurred. This underscores the importance of early detection and awareness among both healthcare providers and patients.
The Elusive Symptoms of Amyloidosis
The symptoms of amyloidosis are notoriously elusive, often mimicking those of other more common diseases. This makes it challenging to diagnose, especially in its early stages. Symptoms can vary widely depending on which organs are affected, but some common signs include fatigue, swelling in the ankles and legs, shortness of breath, and weight loss.
For instance, if the heart is affected, a person might experience symptoms similar to heart failure, such as fluid retention and irregular heartbeat. Kidney involvement can lead to nephrotic syndrome, characterized by protein in the urine and swelling. Gastrointestinal symptoms may include diarrhea or constipation, and in some cases, the tongue may enlarge, a condition known as macroglossia.
Given the broad spectrum of symptoms, amyloidosis can easily be misdiagnosed. This highlights the importance of comprehensive medical evaluation and considering amyloidosis as a potential diagnosis, particularly when symptoms are unexplained or do not respond to standard treatments.
The Importance of Early Detection
Early detection of amyloidosis is essential for several reasons. Primarily, it allows for timely intervention, which can significantly improve the prognosis and quality of life for affected individuals. The earlier amyloidosis is diagnosed, the better the chances of managing the condition effectively and preventing severe organ damage.
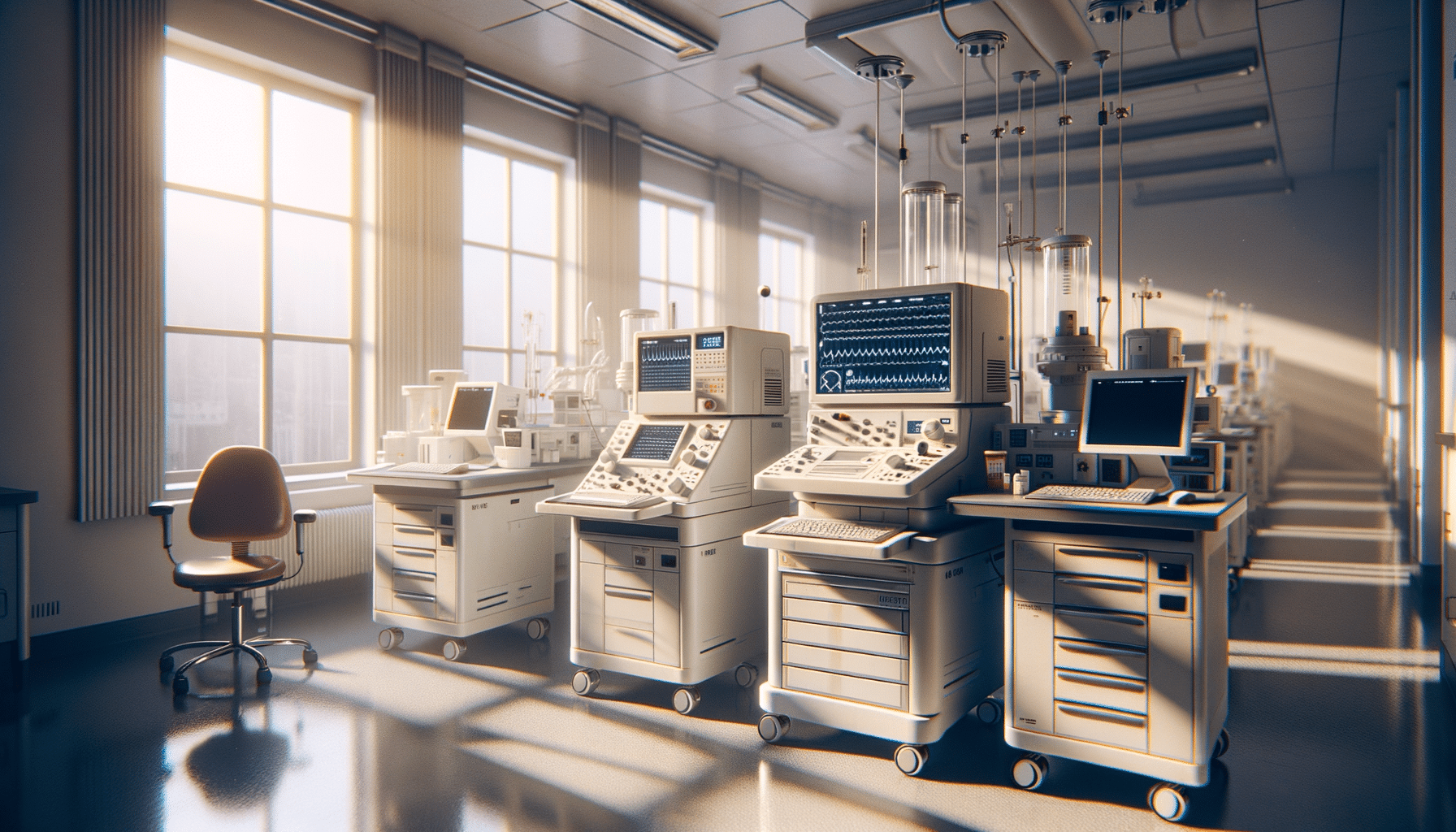
Diagnostic tools such as blood tests, urine tests, and biopsies are crucial in identifying amyloidosis. Advanced imaging techniques and genetic testing can also aid in diagnosis and in determining the specific type of amyloidosis a patient may have. Early detection is not just about diagnosis; it also involves monitoring at-risk individuals, especially those with a family history of hereditary amyloidosis.
Raising awareness about amyloidosis among healthcare professionals and the general public is vital. Educating people about the potential symptoms and encouraging them to seek medical advice if they experience unexplained health issues can lead to earlier diagnosis and better outcomes.
Treatment Options for Amyloidosis
Treatment for amyloidosis depends on the type and severity of the disease. The primary goal is to reduce the production of amyloid proteins and manage symptoms to improve quality of life. For AL amyloidosis, chemotherapy is often used to target the abnormal plasma cells producing the amyloid proteins. In some cases, stem cell transplantation may be considered.
For AA amyloidosis, treating the underlying inflammatory condition is crucial. Medications that help reduce inflammation can slow the production of amyloid proteins. Hereditary amyloidosis may be managed with liver transplantation, as the liver is typically the source of the abnormal protein production.
Supportive treatments, such as medications to manage heart or kidney symptoms, are also important. Lifestyle modifications and dietary changes can help manage symptoms and improve overall health. Collaboration between specialists, including cardiologists, nephrologists, and hematologists, is often necessary to provide comprehensive care.
Conclusion: The Path Forward
Amyloidosis, though challenging to diagnose and manage, can be addressed more effectively with increased awareness and early detection. Understanding the symptoms and having a high index of suspicion can lead to timely diagnosis and treatment, which are crucial for improving patient outcomes.
Continued research and education are needed to enhance understanding of this complex condition. By fostering collaboration among healthcare providers and raising public awareness, we can hope to improve the lives of those affected by amyloidosis and reduce the burden of this often-overlooked disease.